Cataracts are a common vision problem associated with aging. Nearly 70% of individuals over the age of 80 will develop cataracts. In most cases, cataracts begin to form in individuals over 50 and become more common with age. Once cataracts form, they cannot resolve naturally or through medication. Although early cataracts may not need immediate attention, cataract surgery is required once they begin to impair vision. Fortunately, modern cataract surgery is a highly effective and safe procedure that can successfully restore vision.
Cataract surgery is a highly effective outpatient procedure designed to restore clear vision by removing the eye’s clouded natural lens and replacing it with a custom artificial lens. It’s recommended when cataracts begin interfering with daily activities such as reading, driving, or seeing clearly in low light. Modern techniques allow for precise, gentle treatment with minimal discomfort and a relatively quick recovery. Most patients resume normal routines within days, with vision continuing to sharpen over the following weeks.
At Beach Eye Medical Group, cataract surgery is elevated through advanced laser technology, customized lens options, and meticulous preoperative planning to optimize visual outcomes. Led by board-certified ophthalmologist Dr. Shah, Beach Eye combines exceptional surgical expertise, cutting-edge diagnostics, and a patient-first approach to deliver safe, accurate, and consistently outstanding results for patients throughout Orange County.
Every time you look at something, light rays enter your eye via the pupil. The lens focuses this light onto the retina, at the back of your eye. The retina is made up of light-sensitive cells. For the light to be focused correctly, the lens must be clear. If the lens becomes cloudy, this is referred to as cataracts.
The risk of cataracts increases with age. As we age, the lens in our eye thickens, losing both flexibility and transparency. The lens is made up of water and protein. Over time, layers of protein grow on the lens. As these protein layers build up and harden, they cause the lens to cloud.
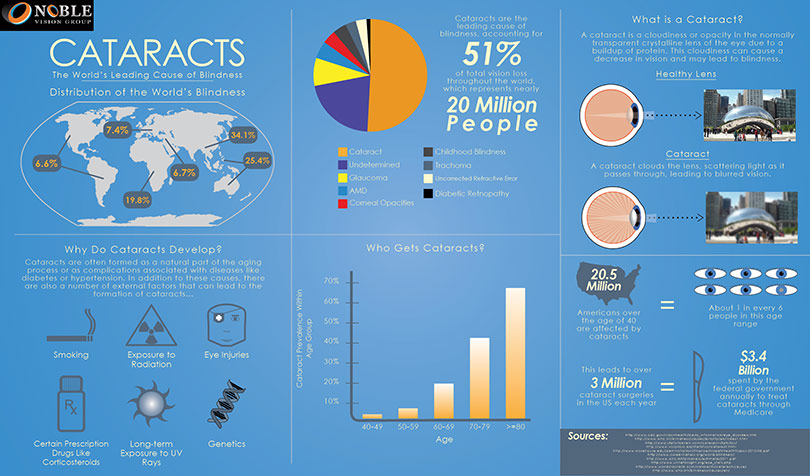
In addition to aging, there are several other factors that increase the risk of cataracts:
If you have cataracts, you may notice that your vision has become blurry, dim, or cloudy. Eventually, this change in your vision could interfere with your daily activities. Cataract symptoms often develop slowly, and you may not notice them at first. Additional symptoms include:
Avoid any eye drops or treatments that claim to dissolve cataracts. These claims are not supported by medical evidence.
There are three other types of cataracts that do not result from aging:
At Beach Eye, cataract surgery is performed by a team of highly skilled ophthalmologists led by Dr. Samir A. Shah, M.D., a board-certified specialist recognized nationally for his expertise and exceptional outcomes. With a complication rate under 0.5%—well below the national average, Dr. Shah brings experience from renowned institutions like UCLA Medical Center and Johns Hopkins Hospital.
Dr. Shah has been repeatedly recognized as one of "America’s Leading Ophthalmologists" by the Consumer Research Council, and is joined by experienced cataract surgeons Dr. Anna Do, Dr. Caleb Shumway, and Dr. Kevin Jwo. Together, they are committed to delivering outstanding visual results.
Our Newport office is accredited by Medicare and the Health Facilities Accreditation Program (HFAP), ensuring high standards of safety, care, and innovation. As a modern ambulatory surgery center, we combine advanced technology—including Corneal Wavefront Refraction—with personalized treatment to help restore your vision with confidence.
If you think you have cataracts, schedule an eye exam with an ophthalmologist. An eye exam will determine whether you have cataracts or another vision problem. You should get your first cataract exam at the age of 40, even if you don’t suspect cataracts. Early detection is essential for protecting your vision. After age 40, get checked every two years; after age 65, get an annual check-up. If your ophthalmologist determines that you do have cataracts, he’ll monitor your vision to see if it gets progressively worse.
Am I Too Old For Cataract Surgery?Here are some common exams ophthalmologists use to diagnose cataracts:
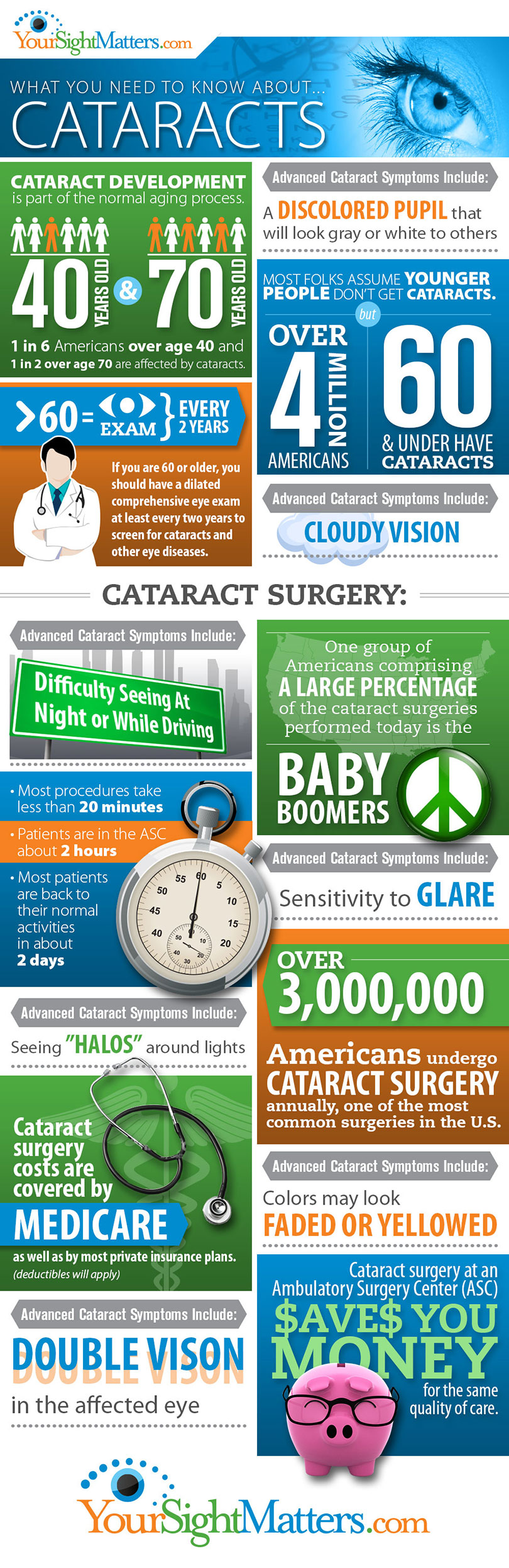
Ophthalmologists may recommend cataract surgery when vision loss due to cataracts significantly affects daily life. The surgery involves removing the clouded lens and replacing it with a clear intraocular lens (IOL). The procedure is outpatient and does not require an overnight hospital stay.
Learn More About The Surgical ProcedureBefore the surgery, our ophthalmologists will perform a comprehensive health assessment of your eyes. It serves as an opportunity for the eye specialist to detect any risk factors that you may have in undergoing the surgery. A full eye evaluation and risk factor assessment are required before going in for surgery.
We may perform a refraction to determine nearsightedness, farsightedness, or any signs of astigmatism prior to surgery. This will be followed by accurate measurements of your eyes to determine critical factors for cataract surgery including the length of your eyes and your corneal curvature.
You will also discuss the options for intraocular lenses that you can choose from. Depending on whether you want to continue using your eyeglasses after surgery or not, our specialist will guide you in selecting the ideal IOL for your needs. You should also take this opportunity to review what other medications you use, particularly if you use any blood thinners or Flomax.
Phacoemulsification is the most common type of cataract surgery. While Dr. Shah personalizes each surgery to the specific needs of the patient, a typical procedure at Beach Eye looks like this:
After cataract surgery, your eye doctor may prescribe antibiotic eye drops for two days to prevent infection. You’ll wear an eye shield immediately following surgery and then while you sleep for several nights. Avoid rubbing your eyes while you’re healing. For your first week of recovery, avoid any strenuous activity as well as getting dirt, dust, or water in your eye. It’s normal to have blurry vision for up to a few weeks after surgery.
Book Your Cataract Surgery Consultation TodayAt Beach Eye, we use advanced laser technology for most cataract surgeries, enhancing precision and outcomes compared to traditional methods. Here’s how laser surgery works:
Laser cataract surgery has revolutionized precision and reliability in vision correction. As technology advances, Beach Eye remains committed to offering the most cutting-edge techniques for optimal patient outcomes.
| Customized Solution | Indications | |
| Recommended IOL | Toric lenses | Multifocal IOL |
| Revisions during surgery | Limbal relaxation incisions may be made alone or combined with implantation of Toric lenses | No additional revisions required |
| Glasses after surgery? | Reading glasses may still be required | Many patients will no longer require prescription lenses |
At Beach Eye Medical Group, we are proud to provide advanced lens options designed to enhance vision and improve outcomes after cataract surgery. Our selection of innovative intraocular lenses ensures each patient receives a solution to their visual needs.
If you are healthy, your cataract surgery recovery process should be quick. Statistics show that the vast majority of cataract surgery is highly successful. To ensure that you are back on your feet quickly post-surgery, Dr. Shah will issue some instructions which include:
If you are interested in seeing what your recovery process will look like, you can read more about it in our “What to Expect After Cataract Surgery” blog post.
Cataract surgery is a safe and common procedure that can significantly improve quality of life. However, like any surgery, it carries some risks and complications associated with it.
If you experience complications after cataract surgery, prompt evaluation is crucial. At Beach Eye Medical Group, our expert team specializes in diagnosing and treating complex cataract cases. We also serve as consultants for managing complications that other eye doctors may find challenging. Contact our Huntington Beach office today to schedule an appointment.
Patients diagnosed with cataracts affecting their vision are candidates for cataract surgery. However, in some cases, we may recommend delaying the procedure:
For all other cases, we advise undergoing surgery as soon as cataracts impair vision, as they will only worsen over time.
Yes. Medicare typically covers medically necessary cataract surgery, including removal of the cataract and implantation of a standard intraocular lens (IOL). It also usually covers part of the cost for pre- and post-operative care.
The procedure itself usually takes 10–20 minutes per eye. Including preparation and brief recovery time, most patients are at the surgery center for about 1–2 hours total.
Patients are generally advised to avoid bending at the waist for at least the first few days, as this can increase pressure in the eye. Your surgeon will let you know when it’s safe to resume normal movements, often within a week.
Most surgeons schedule surgery on the second eye 1–3 weeks after the first, allowing time to ensure proper healing and visual stability before proceeding.
Costs vary based on the type of lens chosen and whether laser technology is used. Standard cataract surgery is often largely covered by insurance or Medicare, while premium lenses or advanced techniques may result in additional out-of-pocket expenses.
Initial recovery is quick. Many patients notice improved vision within a few days. Most normal activities can be resumed within a week, while full healing typically occurs over 4–6 weeks.