Glaucoma is a complex condition. The diagnosis and treatment are not always straightforward. With careful evaluation, regular follow-up visits, and diligent treatment in coordination with your ophthalmologist and primary care physician, vision can be preserved.
Glaucoma1 is a condition that leads to progressive optic nerve damage (optic neuropathy) and eventual blindness if it is left untreated. We don’t know the exact cause, but there are many factors that increase the risk for development and progression of glaucoma. Some of these risk factors include age, genetics (family history), elevated eye pressure, thin corneas, previous eye injury, vascular disease (poor circulation), and other systemic conditions such as hypertension (high blood pressure) and diabetes.
The symptoms above indicate a true eye emergency. If you have any of these symptoms, call your ophthalmologist immediately. Unless this type of glaucoma is treated quickly, severe optic nerve damage, and possibly blindness can result.
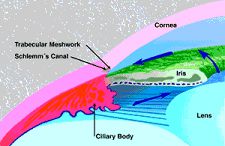
In a normal eye, clear fluid is produced in the ciliary body, behind the iris. This fluid slowly moves to the front of the lens and through the pupil. Eventually it exits the eye through the trabecular meshwork.
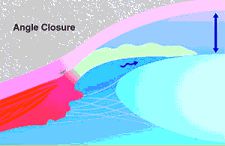
In angle closure glaucoma, fluid can not exit the eye because the trabecular meshwork is blocked by iris tissue. Pressure in the eye can become very elevated, causing damage to the optic nerve.

A laser opening in the iris can provide a bypass route, so fluid can gain access to the trabecular meshwork.
Unfortunately, there is no cure for glaucoma. However, the good news is that glaucoma is one of the most studied diseases of the eye, and many treatment options are available to prevent the progression of glaucoma and preserve the eyesight of patients with the disease. The mainstay of treatment is to optimize the eye pressure for each individual as well as to optimize the patient’s health, especially in regards to cardiovascular disease and diabetes. Your ophthalmologist is the most qualified physician to make recommendations regarding eye pressure control. Some patients may require lower pressures than others. Treatment may include: topical medications (eye drops), oral medications, laser, surgery, or a combination of any or all of these modalities.
Your primary care or family physician will be instrumental in optimizing your overall health, which is also an integral part in the management of glaucoma.
At Beach Eye Medical Group, your ophthalmologist considers many kinds of information to determine your risk for developing the disease.
The most important risk factors include:
Our doctors have years of experience treating glaucoma patients across Orange County and will weigh all of these factors before deciding whether you need treatment for glaucoma, or whether you should be monitored closely as a glaucoma suspect. This means your risk of developing glaucoma is higher than normal, and you need to have regular examinations to detect the early signs of damage to the optic nerve.
There are very few symptoms of glaucoma in the early stages of the disease. Since there is no cure for glaucoma, it is critical to detect and treat glaucoma at its earliest stage in order to preserve the eyesight. By the time a person notices symptoms at home, such as blind spots, difficulty functioning in low-lighting conditions, tunnel vision, or visual loss, it may be too late. These symptoms usually develop slowly over time and may take years to develop, making it even more difficult to notice. Occasionally, a person may experience an acute “attack” of glaucoma, consisting of severe pain, halos, redness, unilateral headache, nausea, and blurry vision. If you experience any of these symptoms, it is an emergency, and you should contact your ophthalmologist urgently.
Otherwise, a screening exam by your ophthalmologist is the most effective defense against glaucoma. If you have a strong family history of glaucoma or blindness, you should be examined in your 20’s. If you have had a serious eye or head injury, you should be examined at the time of your accident and yearly thereafter. All others should have a screening exam before the age of 50. Your ophthalmologist will then make recommendations for future appointments after the initial visit.
At the time of your examination, your doctor may elect to have you return for additional glaucoma testing if it is warranted. These tests include Visual field testing (peripheral vision test), optic nerve imaging, and corneal thickness measurement. It is important to return for these additional tests if your doctor has clinical suspicion, and it should be repeated periodically, at least on an annual basis. Sometimes, a diagnosis may not be possible after the initial visit and may require vigilant monitoring, sometimes over years, before a definitive diagnosis of glaucoma can be made.
A significant benefit of having your glaucoma care4 and follow up performed at Beach Eye Medical Group, Irvine is that we have invested in the most advanced technology to monitor glaucoma progression. We use the Cirrus HD OCT (Optical Coherence Tomography) from Carl Zeiss Meditec. With this instrument, we are able to detect subtle and small changes in the health of your optic nerve better than ever before. Wherever you choose to go, make sure your eye care provider has invested in the best technology for you. Remember, vision loss in glaucoma is not reversible so early detection and treatment is the best therapy.
If your doctor institutes treatment, it is important to comply with all medical therapy and follow-up visits. Again, since there is no cure, prevention is critical.
Glaucoma is a slow-progressing disease. Though it is unlikely that you would go completely blind from glaucoma, uncontrolled glaucoma can certainly lead to progressive vision loss. A certain form of glaucoma known as Narrow-Angle glaucoma may lead to quick vision loss because of the acute nature in which it can present. Your doctor can help decrease the risk of acute vision loss with regular examinations and a laser procedure known as a peripheral iridectomy.
The information contained above is not intended to be a comprehensive discussion of glaucoma, but rather an overview.
Please visit the website of the American Academy of Ophthalmology and The Glaucoma Research Foundation for additional information: To discuss your eyesight with a specialist, book a consultation at Beach Eye Medical Group, Irvine 714-965-9696
References
1 Glaucoma. Available: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma
2 Chronic open-angle glaucoma. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479464/
3 Acute Closed Angle Glaucoma. Available: https://www.ncbi.nlm.nih.gov/books/NBK430857/
4 What Is Glaucoma? Symptoms, Causes, Diagnosis, Treatment. Available: https://www.aao.org/eye-health/diseases/what-is-glaucoma
Fantastic for pinguecula removal. Dr Shah is amazing and he has helped me remove pingueculas from both eyes. He is so friendly and reassuring. This has been twice I have come here and it has been a wonderful experience!