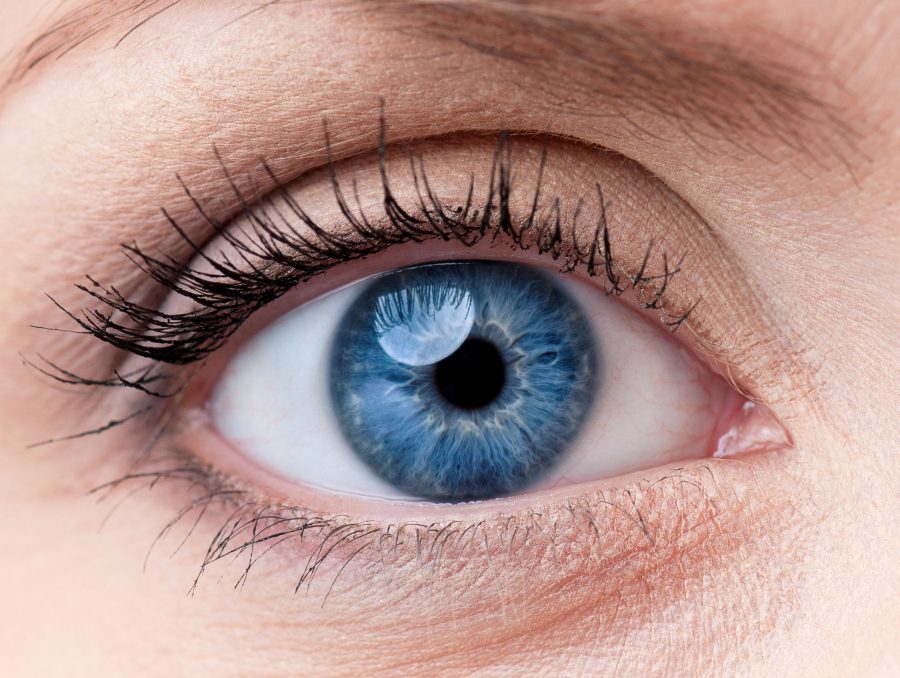
Every time you look at something, light rays go into your eye via the pupil. The lens focuses the light onto the retina at the back of your eye. The retina is made up of a layer of light-sensitive cells. For the light to be focused properly, the lens has to be clear. If the lens is cloudy, this condition is called cataracts.
The risk of cataracts1 increases as you get older. 70% of people who are 75 years old have cataracts. As we age, our eye’s lens becomes thicker, losing flexibility and transparency. The lens is made from water and protein, and protein layers continue to grow on the lens. When protein builds up on the lens, clumps together, and hardens, the lens becomes cloudy.
Aside from aging, there are other factors that increase your risk of getting cataracts:
If you have cataracts, you may notice that your vision has become blurry, dim, or cloudy. Eventually, this change in your vision could interrupt your daily life. Since most cataracts develop with age, cataract symptoms are not always noticeable at first. Additional symptoms include:
While some eyedrops claim to “dissolve” cataracts, this isn’t possible. Avoid any treatments that claim to fix or remove cataracts.
While rarer, there are three other types of cataracts2 that don’t occur due to the natural aging process:
If you think you might have cataracts, visit an ophthalmologist. An eye exam will determine if you have cataracts or another vision problem. At the age of 40, you should get your first cataracts exam, whether you suspect you have it or not. Early detection is the key to protecting your vision. Get checked every two years thereafter. After the age of 65, get checked annually for cataracts.
If your ophthalmologist determines that you do have cataracts, he’ll monitor your vision to see if it gets progressively worse. The only way to treat cataracts is through surgery, but many people find that their vision improves simply with a new eyeglass prescription. If the clouding is mild or is only on a small portion of your eye’s lens, you may not need surgery to improve your vision.
There are a few different ways for an ophthalmologist to diagnosis cataracts:
Ophthalmologists often suggest cataract surgery for people with severely-affected lenses and whose vision loss is greatly affecting their day-to-day life. During cataract surgery, the eye’s natural, the clouded lens is removed and replaced with a clear, artificial lens implant – an intraocular lens or IOL. This surgery is an outpatient procedure and does not require an overnight stay in the hospital.
Before undergoing surgery, an A-scan is used to measure the length of your eye. Keratometry is a technique that’s used to measure the curve of your cornea. These measurements help your eye doctor to choose the right lens implant for your eye.
Phacoemulsification is the most common type of cataracts sugary. A small incision is made to the side of the cornea. An instrument that uses high-frequency ultrasound is inserted, breaking up the center of the lens and suctioning it out. Then, the IOL is inserted either behind or in front of the iris. The incision is closed, sometimes without the use of stitches.
Patients who have had vision correction surgery, like LASIK3, should provide their ophthalmologist with the vision correction prescription from before their surgery. This will help your doctor to figure out the right IOL prescription. You should also tell your doctor about any medications and nutritional supplements you’re taking.
After cataracts surgery, your eye doctor may prescribe antibiotic eye drops for two days to prevent infection. You’ll wear an eye shield immediately following surgery and then while you sleep for several nights. Avoid rubbing your eyes while you’re healing. For your first week of recovery, avoid any strenuous activity as well as getting dirt, dust, or water in your eye. It’s normal to have blurry vision for up to a few weeks after surgery.
References
1 Cataracts. Available: https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
2 What Is a Cataract? Available: https://www.healthline.com/health/cataract
3 LASIK. Available: https://www.aao.org/eye-health/treatments/lasik
Written by Dr. Shah
I was pleasantly surprised as this was my first visit, referred by my PCP. I was greeted by their very competent and efficient Ophthalmology Assistant, who also provided theatrical comic relief. : ^ } Due to COVID, all were following proper protocol. The diagnostic tools were state-of-the-art, and Dr Jwo was pleasant and competent!